Table of Contents
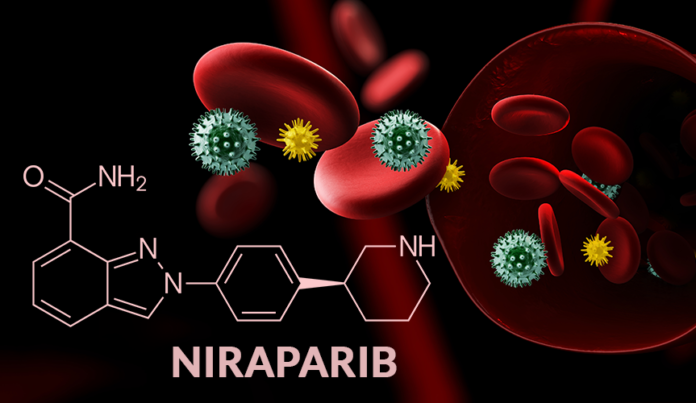
What is Niraparib?
Niraparib is a medication used to treat certain types of ovarian, fallopian tube, and primary peritoneal cancer. PARP inhibitors are the class of drugs for Niraparib. It works by blocking an enzyme called PARP, which repairs DNA damage. By blocking PARP, Niraparib causes cancer cells to die.
It’s important to mention that the production of Niraparib API must comply with the regulations of each country, the WHO, and the FDA, among others, to guarantee the API’s quality, efficacy, and safety.
Niraparib API is then formulated into a finished dosage form, such as tablets or capsules, for patient distribution and use. The finished dosage form may include other ingredients such as fillers, binders, and coatings.
Niraparib is chemically known as:-
(S)-N-(3-((3-aminopyridine-2-carbonyl)amino)phenyl)-3-((4-(4-chloro-3-(trifluoromethyl)phenyl)-1,2,4-triazol-1-yl)methyl)benzamide. It can be recognized as a white to off-white powder, which is soluble in methanol and ethanol, and slightly soluble in water.
Formula: C19H20N4O
ChEMBL Id: 1094636
ChemSpider ID: 24531930
Pronunciation: /nɪˈræpərɪb/; nih-RAP-uh-rib
Protein binding: 83%
Other names: MK-4827
Metabolism: Carboxylesterases
Some Significant Niraparib Uses
Niraparib API is approved as a maintenance treatment for adult patients suffering from epithelial ovarian, fallopian tube, or primary peritoneal cancer. Patients with an incomplete or partial response to platinum-based chemotherapy are also prescribed this drug. Some other major uses of Niraparib are:
- Maintenance treatment of adult patients who are suffering from deleterious or suspected deleterious germline BRCA-mutated (gBRCAm) recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer who have been treated with three or more prior lines of chemotherapy.
- It can be used to treat adult patients with relapsed small cell carcinoma of the ovary, hypercalcemic type (SCCOHT), who have received at least two prior lines of therapy.
What are the Major Niraparib Side Effects?
It is important to note that Niraparib treatment should always be taken under the supervision of a qualified oncologist. The physician will evaluate the benefits and risks of the treatment for each patient and will monitor the patient’s response to the treatment, and adjust the dosage accordingly. But, like all medications, it can cause side effects. Some common side effects of Niraparib include:
- Nausea
- Fatigue
- Anemia
- Thrombocytopenia (low platelet count)
- Vomiting
- Diarrhea
- Constipation
- Loss of appetite
- Headache
More serious side effects of Niraparib include:
- Blood clots
- Severe bleeding
- Myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML)
- Tumor lysis syndrome (TLS)
- Embryo-fetal toxicity
If you experience any kind of side effects while taking Niraparib, it is crucial to inform your healthcare provider. They might adjust your dosage or recommend ways to manage the side effects.
Precautions of Niraparib that You Should be Aware Of
Niraparib is a medication used to treat certain types of ovarian, fallopian tube, and primary peritoneal cancer. It is important to take certain precautions when using Niraparib. Some precautions to be aware of include the following:
- Blood clotting: Niraparib may increase the risk of blood clots. Your healthcare provider may monitor your blood clotting function more frequently while taking Niraparib.
- Bleeding: Niraparib may increase the risk of bleeding. Your healthcare provider may monitor your blood clotting function more frequently while taking Niraparib and may recommend measures to reduce the risk of bleeding.
- Myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML): Niraparib can cause MDS and AML. Your healthcare provider will monitor your blood counts while taking Niraparib, and you may discontinue the medication if these conditions develop.
- Tumor lysis syndrome (TLS): Niraparib can cause TLS. Your healthcare provider will monitor you for the signs and symptoms of TLS and may take measures to prevent or treat the condition.
- Pregnancy and breastfeeding: Niraparib can cause harm to a developing fetus. Women who have reproductive potential should use effective contraception during their treatment and should continue for at least six months after the last dose of Niraparib. Women should not breastfeed while taking Niraparib.
- Interactions with other medications: Certain medications may interact with Niraparib, so it is significant to give information about all medications, vitamins, and supplements you are currently taking before starting Niraparib treatment with your healthcare provider of
Who Should Not Take Niraparib?
There are certain individuals who should not take Niraparib or who should use it with caution. These include:
- Individuals who are pregnant or planning to become pregnant, Niraparib can cause harm to a developing fetus.
- Individuals who are breastfeeding, such as Niraparib, may pass into breast milk and may cause harm to a nursing infant.
- Individuals with a history of blood clots or bleeding disorders, such as Niraparib, may increase the risk of blood clots and bleeding.
- Individuals taking other medications may have a higher risk of bleeding, such as warfarin or aspirin.
- Individuals who have or had bone marrow disorders such as Niraparib can cause Myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML)
- Individuals who have or had tumor lysis syndrome (TLS)
- Individuals who are allergic to Niraparib or any of its ingredients.
How does Niraparib work to Treat Different Types of Cancer?
Niraparib works by inhibiting the activity of an enzyme called poly(ADP-ribose) polymerase (PARP), which is involved in repairing DNA damage in cells. When PARP is inhibited, the cancer cells are unable to repair their DNA and eventually die. This mechanism of action is particularly effective in cancer cells with mutations in genes involved in DNA repair, such as BRCA1 and BRCA2.
DNA of Cancer cells often has, which makes them more dependent on PARP for survival. By inhibiting PARP, Niraparib causes cancer cells to die, while leaving normal cells relatively unharmed.
In the case of BRCA-mutated cancer, the BRCA1 and BRCA2 genes are responsible for the repair of DNA double-strand breaks. When these genes are mutated, the cells are unable to repair the DNA damage properly, so the PARP inhibitors like Niraparib can take advantage of this vulnerability and cause cancer cell death.
Conclusion
Niraparib active pharma ingredient typically use synthetic chemical processes. The raw materials used in the synthesis of Niraparib include various chemicals such as amino acids, organic acids, and solvents. These raw materials are combined and reacted in a series of steps to produce the final API.
Talking to your healthcare provider is vital before starting Niraparib treatment, especially if you have a history of blood clots or bleeding disorders or in case you are on any other medications that may increase the risk of bleeding.