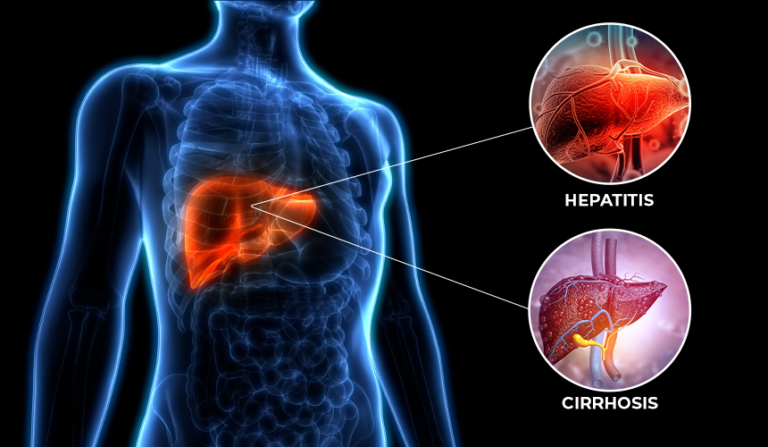
The liver detoxifies metabolites, synthesizes proteins, and produces different chemical compounds necessary for digestion in order to function properly.
A person’s ability to carry out normal liver functions is disrupted by hepatitis and cirrhosis.
Cirrhosis is liver scarring that remains indefinitely, often caused by chronic hepatitis. Hepatitis generally is reversible (curable); cirrhosis is not. Unlike hepatitis, which can develop quickly in some cases, cirrhosis also takes time to develop.
By reviewing the basic symptoms of both diseases and then identifying their main similarities, we can better understand both.
About Hepatitis and Cirrhosis
Hepatitis
Hepatitis can be classified into a number of types. Chronic or acute hepatitis causes inflammation and eventually damage to the liver tissue due to a viral infection of the liver. Food and water contaminated with pathogens are responsible for the spread of hepatitis A and E. Infection with hepatitis B is transmitted by direct contact with the bodily fluids of an infected person, such as blood or semen. Blood-borne hepatitis C is transmitted by sharing needles with someone infected. Infectious blood contact with someone with hepatitis B causes hepatitis D, which cannot be transmitted without hepatitis B.
Symptoms:
- Fatigue
- Flu-like symptoms
- Pale stool
- Dark urine
- Abdominal pain
- Appetite loss
- Unexpected weight loss
- A yellow complexion and yellow eyes may indicate jaundice.
Cirrhosis
Cirrhosis causes the liver to proliferate and scar as it increases connective tissue production, distorts the blood flow architecture, and ultimately results in liver necrosis. The condition had been thought to be irreversible at the time of diagnosis. However, reversing the fibrosis (the generation of “stiff” connective proteins) that causes liver cirrhosis can be accomplished if the underlying cause is corrected.
Symptoms:
- Fatigue.
- Bruising or bleeding easily.
- The inability to eat.
- Nausea.
- Ankle, foot, or leg swelling (edema)
- Weight loss.
- Itchy skin.
- Skin and eye discoloration (jaundice)
Link Between Hepatitis and Cirrhosis
Cirrhosis can be caused by Hepatitis C, but cirrhosis cannot be caused by hepatitis C. To get hepatitis C, an individual has to be exposed to the virus. When people come into contact with the blood of someone with hepatitis C, they are likely to contract the virus.
The following methods can be used for transmission:
- Needle sharing
- Injuries caused by needlesticks among healthcare workers
- Engaging in sexual activity
- Hepatitis C transmission from a parent
Additionally, it is possible to be infected with hepatitis C for a long time without being aware.
Statistics suggest that about 15 to 25 percent of people who contract hepatitis C will experience this. Chronic infections may affect the remainder. In the early stages of infection, people usually experience mild illness, and their bodies may completely clear the virus.
Often, chronic hepatitis C causes cirrhosis, leading to liver scarring.
Cirrhosis can also be caused by the following:
- Addiction to alcohol or liver disease caused by alcohol
- Immune-mediated hepatitis, where the immune system attacks the liver
- The chronic condition of heart failure
- Viral hepatitis, chronic hepatitis B
- Liver diseases caused by inheritance
- Type 2 diabetes
The liver filters and processes toxins and creates essential proteins for the body. A liver damaged by cirrhosis may not be able to function as well, which could lead to its failure.
Symptoms of Cirrhosis due to Hepatitis C
Symptoms of liver cirrhosis may not appear until a great deal of damage is done to your liver, making them difficult to notice. Symptoms that you may experience include the following when you experience symptoms:
- Fatigue
- Nausea
- Loss of appetite
- Weight loss
- A tendency to bleed or bruise easily
- Skin itching
- Skin and eye discoloration (jaundice)
- Inflammation of the legs
- An abdominal fluid collection (ascites)
- Testing abnormalities in bilirubin, albumin, and coagulation parameters
- Vascular bleeding may occur in the esophagus and upper stomach due to enlarged veins.
- Toxin buildup in the brain (hepatic encephalopathy) impairs mental function.
- Bacterial peritonitis is the infection of the abdominal cavity lining and ascites.
- The combined failure of the kidneys and liver (hepatorenal syndrome)
In people with HCV who undergo a liver biopsy, scarring will be visible, confirming that cirrhosis has occurred in their bodies. You may not need to undergo a biopsy if your doctor performs lab tests and conducts a physical examination.
Read Also: What Are the Various States of Hepatitis B?
Medication used to Treat Hepatitis and Cirrhosis
Consult your doctor about the best way to prevent further damage to the liver caused by hepatitis C and cirrhosis. Alcohol consumption, for instance, can damage the liver.
There are a number of medications by pharmaceutical ingredients manufacturers that pass through the liver, which is why you should consult your doctor if you take any of the following medications that may negatively affect the liver:
- Herbs
- Prescription pills
- Other medications
- Supplements
Doctors may prescribe medications for the treatment, such as Tenofovir Alafenamide Fumarate, Velpatasvir, Ledipasvir, and Daclatasvir dihydrochloride.
- The medication tenofovir belongs to a class of medication known as nucleoside reverse transcriptase inhibitors (NRTIs). Essentially, they suppress the immune response by lowering the amount of hepatitis B virus in the blood. Hepatitis B cannot be cured, complications of the disease like cirrhosis of the liver or liver cancer cannot be prevented, and the virus cannot be transmitted.
In some cases, tenofovir is very effective at treating hepatitis B. Adefovir and lamivudine are often less successful than tenofovir in some situations. Several studies have indicated that tenofovir is an effective long-term treatment for HBV, particularly for people with lamivudine resistance.
No clinically relevant bone loss and few kidney-related side effects have been reported.
- An effective and well-tolerated option for treating chronic hepatitis C (HCV) infection is the fixed-dose combination of ledipasvir-sofosbuvir taken once a day. Hepatitis C was treated with this direct-acting antiviral regimen for the first time without interferon or ribavirin from the FDA. Patients with genotype 1A who are not cirrhotic and experienced with treatment can use ledipasvir-sofosbuvir without ribavirin.
- As a dual therapy, sofosbuvir plus velpatasvir is highly effective and safe for treating patients with genotypes 1, 2, 3, 4, 5, and 6 of the hepatitis C virus in conjunction with advanced fibrosis or compensated cirrhosis. Hepatitis C patients have been treated with interferon-based treatments. In the treatment of chronic HCV infections, sofosbuvir and velpatasvir are used in combination.
Defosbuvir-velpatasvir is a once-daily combination pill of sofosbuvir 400 mg and velpatasvir 100 mg. With or without food, one tablet is recommended once daily.
-The dosage should not be adjusted in patients with any degree of renal impairment, including patients on dialysis for end-stage renal disease. Data from mostly observational studies were used to update the recommendations for dosing in persons with renal impairment.
-Hepatic Impairment: Sofosbuvir-velpatasvir dosage does not need to be adjusted in patients with mild, moderate, or severe hepatic impairments (Child-Pugh Class A, B, or C). Patients with decompensated cirrhosis who receive sofosbuvir-velpatasvir and ribavirin should be monitored clinically and in the laboratory.
- Daclatasvir is now being tested for people awaiting or undergoing liver transplants with chronic hepatitis C. Cirrhosis patients can take daclatasvir if they suffer from compensated liver disease. The drug, however, is more effective in people with less advanced liver damage. Daclatasvir is now being tested for people awaiting or undergoing liver transplants with chronic hepatitis C.
A sustained virologic response is usually achieved by 95% to 99% of patients without cirrhosis or with compensated cirrhosis (defined as less than 15 IU/mL of HCV RNA at 12 weeks after completion of treatment; sustained virologic response is merely a biomarker of a cure for HCV infection but does not necessarily mean a direct effect on morbidity or mortality). It has been shown that patients with HCV genotypes 1, 2, 4, 5, and 6 receiving sofosbuvir/velpatasvir achieve sustained virologic responses compared to patients with placebo (n = 116) in one small study. The patients treated with a placebo were not successful.1,3 For HCV genotype 3, sofosbuvir/velpatasvir has a 95% response rate compared to sofosbuvir/ribavirin, with an 80% response rate.1,4. The patients treated with a placebo were not successful.
A 94% sustained virologic response will be achieved in decompensated cirrhosis patients (Child-Pugh score B) when sofosbuvir/velpatasvir and ribavirin are combined. Neither elbasvir/grazoprevir nor ledipasvir/sofosbuvir nor sofosbuvir/velpatasvir have been studied to compare their effectiveness.
Conclusion
Many similarities exist between hepatitis and cirrhosis, but they only exist on a continuum rather than in opposition. As good medical care and proper medication by trusted active pharmaceutical ingredient manufacturers are provided in the early stages of liver inflammation that leads to cirrhosis, many of the causes can be reversed with good medical care.